A Clemson University researcher has revealed previously unknown information about how bacteria and fungi interact in the lungs of people with cystic fibrosis (CF).
CF, one of the most common genetic diseases in the United States, causes an abnormally sticky, thick mucus to build up in the lungs, providing the perfect breeding ground for infections.
Two of the most commonly found microbes in the lungs of people with CF are Pseudomonas aeruginosa, an opportunistic bacterium that causes invasive and life-threatening infections in the immunocompromised, and Aspergillus fumigatus, a common fungus whose spores most people breathe in every day without getting sick. This fungus can also cause serious illnesses in people with weakened immune systems.
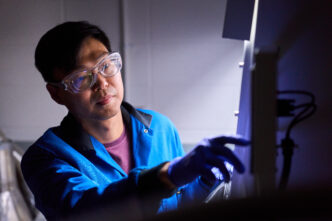
Stephen Dolan, an assistant professor in the Department of Genetics and Biochemistry, and his collaborators from Georgia Tech uncovered how the two organisms interact molecularly in the lungs they infect.

“Cystic fibrosis results in a wide range of challenging symptoms which impact the entire body, but repeated lung infections leading to lung damage is the major cause of mortality. It’s mostly bacteria and fungi like Pseudomonas and Aspergillus which are responsible for these infections. And, a lot of times, they infect together and cause very serious issues,” said Dolan, who conducts his research at the Clemson University Eukaryotic Pathogens Innovation Center (EPIC).
Dolan’s research focuses on microbial interactions in human infections and in the environment. He became interested in studying respiratory infections in CF patients during his Ph.D. at Maynooth University in Ireland, a country that has the highest rate of CF per capita in the world.
“Everybody at home knows somebody affected by CF because it’s so prevalent,” said Dolan, who said his CF-related research allows him to do high-level microbiology that is also clinically relevant.
Microbes rarely exist in isolation. Because they must live — and survive — in complex polymicrobial communities, they develop intricate offensive and defensive strategies that enhance their fitness in the competitive environment.
Co-existing
Dolan uncovered a previously unknown toxin detection system that allows P. aeruginosa to see and respond to toxins produced by A. fumigatus, permitting the two microbes to co-exist in the sputum in CF lungs.
Using a preclinical model mimicking expectorated human CF sputum, the researchers found that when P. aeruginosa was exposed to A. fumigatus, it activated a previously uncharacterized gene, PA4170. Upon further analysis, they uncovered that PA4170 encodes an enzyme that protects P. aeruginosa from a toxin produced by A. fumigatus. It is the same mechanism which the fungus uses to protect itself from being harmed by the toxin it produces.
“It appears that ecologically, over millions of years, these microbes have been growing together in soil and have developed elaborate strategies to compete for space and nutrients, and then when they get into humans, those in-built mechanisms have allowed them to coexist and cause serious infections,” he said. “It’s like a marriage of convenience in the sense that most other microbes can’t occupy the same niche alongside these pathogens, but they’re able to withstand each other.”
Dolan said the discovery could lay the groundwork for more effective treatment and detection of polymicrobial lung infections in people with CF.
Dolan recently received a Career Transition Award (K22) from the National Institute of Allergy and Infectious Diseases (NIAID) to continue research on fungal-bacterial interactions in human infection. His research is also supported by the Cystic Fibrosis Foundation.
Detailed findings were published in the journal The Proceedings of the National Academy of Sciences (PNAS) in an article titled “Convergent evolution in toxin detection and resistance provides evidence for conserved bacterial-fungal interactions.”