Doctors, nurses and patient care technicians have incredibly important jobs. They relieve suffering, nurture people back to health and literally save lives.
It’s no question they should have the highest quality education, but some of their skills have been taught the same way for years, even though technology offers new opportunities for enhanced learning.
For Joseph Singapogu of Clemson University, the gap was an opportunity.

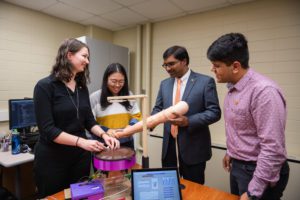
Singapogu, an assistant professor of bioengineering, works with a team of graduate students and collaborators from around the country to develop new simulators aimed at taking medical education to the next level.
The simulators are outfitted with cameras and sensors to collect data that provide students and their instructors with meaningful metrics about how well they are learning the skills they need to treat patients effectively.
Among those simulators is one that would help vascular surgeons learn to suture blood vessels and two that could help patient care technicians find fistulas, the vein-and-artery combination that serves as lifelines for dialysis patients.
“Our work could result in real, tangible impact to patients,” Singapogu said. “If patient comfort is increased and medical errors are decreased, that’s what motivates me and I think a lot of my students. It’s very rewarding work.”
Singapogu’s team has received two grants from the National Institutes of Health totaling more than $1.8 million to support its work. All the simulators are designed to complement, not replace, human instruction.
Watch this video and read the text below it to learn more:
CanSim
The challenge: Surgeons create fistulas in patients with kidney failure so that large amounts of blood can be withdrawn, treated in a dialysis machine and returned to the patient. A fistula is created when an artery and vein are surgically connected, usually at the wrist or the forearm. The difficulty for technicians is that fistulas can be difficult to find when buried beneath a patient’s flesh. Technicians need to find the fistula to insert the cannula, a needle that connects the patient to the dialysis machine.
Mistakes can cause pain for the patients, ruin the fistula and require a catheter that raises the risk of infection. And none of this is cheap. Hemodialysis costs about $35 billion in the United States annually, paid almost entirely by Medicare, said Prabir Roy-Chaudhury, a Singapogu collaborator and professor of medicine in the Division of Nephrology and Hypertension at the University of North Carolina School of Medicine.
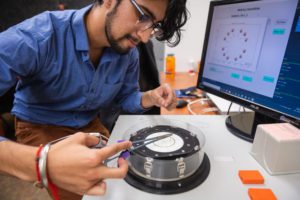
What CanSim does: The prototype simulator that the Singapogu team has developed is round and about the width of a medium pizza. A sheet of cured silicone that simulates the flesh is laid over tubes that are spaced out on a platform and simulate fistulas. The same kind of motor that makes cell phones buzz simulates vibration caused by blood flow in an actual fistula. The idea is to help technicians master the ability to find the fistula so they can effectively insert the cannula. CanSim helps students understand how gently or firmly they are holding the wings of the needle. The simulator also tracks the motion of the needle and several other aspects of student performance.
What collaborators say:
“Joseph has identified cannulation as the weakest point in this $35-billion hemodialysis enterprise, and he is trying to develop a system that is going to train these cannulators in doing a better job. I think his simulator should be in every dialysis unit.”
Prabir Roy-Chaudhury, a professor of medicine in the Division of Nephrology and Hypertension at the University of North Carolina School of Medicine
Sonavex
The challenge: One of Singapogu’s collaborators, Sonavex, has developed an ultrasound-based, smart guidance system for inserting needles. Sonavex wanted to ensure that its device was properly coaching its users on needle insertion, so the Baltimore-based company approached the Singapogu team to see if it could measure how well nurses and technicians insert the cannula.

The Singapogu team is developing an echogenic device that provides an objective assessment of how well cannulation is performed. The device will provide visual feedback from the ultrasound and generate metrics to rate the quality of needle insertion.
The potential: Some fistulas are exceptionally hard to locate beneath the flesh. An ultrasound device could provide a visual way of finding those fistulas and inserting the cannula in the right place.
What collaborators say: “Joseph has built a state-of-the-art cannulation simulator device that will be instrumental in improving cannulation for dialysis patients. Cannulation injuries are incredibly common and cause substantial patient morbidity and healthcare costs. Joseph’s technology has the potential to dramatically improve cannulation through both training of patient care technicians and by providing a mechanism to validate novel cannulation technologies. Joseph has been the perfect collaborator and our team is thrilled to work with him and his team.”
David Narrow, CEO of Sonavex
SutureCoach
The challenge: Vascular surgeons have to perform delicate operations to suture together blood vessels. A slight motion in the needle can result in a mistake that causes blood leakage.
What SutureCoach does: Students test their skills on a flat surface about the size of a salad plate. The device comes equipped with sensors and cameras to provide a wide range of metrics on suturing skill, including the motion of the needle and the wrist. SutureCoach would be useful for anyone interested in becoming a vascular surgeon, Singapogu said. Suturing is a common skill for surgeons, so the device could also prove useful for general surgery, he said.
Part of the research focuses on how to rate the user’s performance relative to others and how well the rating predicts outcomes for patients, said Richard Groff, a Clemson associate professor of electrical and computer engineering who is collaborating on the project. “The piece of the puzzle that is most interesting to me is how we can take these data streams we are getting from the simulator and provide automatically generated instructions that help trainees improve performance,” Groff said. “This is a specific instantiation of a general problem, but one where we have an opportunity to make an impact.”
What collaborators say: “I felt this was a step in the right direction. What Dr. Singapogu’s project really attacks is how we get objective metrics, what we look at and how we figure out what the standard is. His project really intrigued me in the sense that we’re able to objectively look at ourselves and figure out how we can be better.”
Sagar Gandhi, a vascular surgeon at Prisma Health and a clinical assistant professor with Clemson University School of Health Research
Who is Singapogu?
Singapogu came to Clemson for his Ph.D. in bioengineering, which he received in 2012. He then worked as an embedded scientist at Prisma Health. “During that time, I was fortunate to shadow surgeons and nurses, and that gave me the opportunity to come face to face with the problems they were facing,” he said. Many of Singapogu’s projects result from real-world challenges. The idea for the CanSim, for example, originated with a cab ride he shared with a renowned vascular surgeon and nephrologist who were talking about cannulation problems.
What do Singapogu’s collaborators say about their work together?
“With the amount of information we get from these simulators, they will be fantastic educational tools. It’s a matter of streamlining the process. When this is all said and done, in real time people will get immediate feedback the moment they get done working with the simulators.”
Joseph Bible, a Clemson University assistant professor of mathematical and statistical sciences, who is helping the research group translate data into information meaningful to the simulators’ users
Why is Clemson a good place for this work?
“Clemson is an amazing place, because we are uniquely positioned in South Carolina. We have a great bioengineering department. In addition, the ecosystem of engineering here affords collaborations very easily. For instance, on my projects, we collaborate with industrial engineers, electrical engineers and clinicians in Greenville, Charleston and North Carolina. In addition to that, I also think we in South Carolina are able to work on public health problems that other parts of the U.S. might not necessarily see.”
Joseph Singapogu
What do students think about studying under Singapogu?
“What I like best about our research is that it’s meaningful. It’s going to impact patients’ lives. The fact that it’s going to reduce someone’s pain, that means a lot.”
Mehdi Shayan, Ph.D. student
“It’s going great. Coming into this year, I can really look back to when I first got here and how much I’ve improved on almost every aspect of my work– how I approach problem-solving, how I can code and how I can solve research problems.”
Simar Singh, fourth-year Ph.D. student who hopes to work with a robotics prosthetics company after graduation
“I like that the work is a little bit of everything. I really like that it’s hands-on, because I’m very much a hands-on person. Theory is great and all, but if it can be applied, that’s way better.”
Lydia Petersen, a third-year Ph.D. student whose work on the CanSim includes leading development of the blood flashback system and working on visual feedback capabilities
“He’s always patient with me. English is my second language. At the beginning, if I didn’t understand something, he would write down what he said so I could understand what he meant. He always says, ‘If you have any confusion, come to my office.’”
Ziyang Zhang, Ph.D. candidate
“‘Work on multiple projects.’ That’s what the professor keeps telling us. Multiple projects help us develop lots of skills…. My professor and lab mates are really great. I’m really enjoying my time here.”
Devansh Shukla, a master’s student who is working on the CanSim and on the Sonavex collaboration
What do the college’s administrators say about Singapogu’s work?
“Dr. Singapogu’s close collaboration with medical professionals ensures that his team’s innovations are helping solve real-world challenges. He is uniquely positioned to have an impact on health innovation nationwide.”
Martine LaBerge, chair of the Department of Bioengineering
“Dr. Singapogu has built a team of collaborators and students who are working together to advance health innovation in South Carolina and beyond. The grants he has received are a testament to the scholarship he brings to Clemson. By helping create better doctors, nurses and technicians, they are helping create healthier patients.”
Anand Gramopadhye, dean of the College of Engineering, Computing and Applied Sciences
Get in touch and we will connect you with the author or another expert.
Or email us at news@clemson.edu

