CRISPR is a powerful gene-editing technology that research scientists use to selectively modify the DNA of living organisms so they can study gene function in disease, develop diagnostic tests and identify novel treatments.
CRISPR, short for Clustered Regularly Interspaced Short Palindromic Repeats, was discovered in bacterial immune systems. When a virus attacks, bacteria save tiny pieces of the viral DNA. The next time the virus appears, the bacteria use CRISPR and a protein called Cas9 to locate and destroy the invader’s DNA. Scientists discovered they could copy the mechanism by designing custom guide RNAs that leads CAS9 to the exact spot in human, plant or animal DNA they want to edit.
World CRISPR Day — which is celebrated on October 20, the day CRISPR was first used to edit a human genome — was established to celebrate its transformative impact on science, medicine and biotechnology.
Here is how three Clemson University scientists use CRISPR in their research to advance human health.

Stephen Dolan
Stephen Dolan, an assistant professor in the Department of Genetics and Biochemistry, uses CRISPR to better understand fungi that infect the human respiratory tract. His research focuses on uncovering the genetic mechanisms that allow these organisms to grow, adapt and resist treatment, insights that could ultimately inform new antifungal therapies.
Dolan uses CRISPR technology to “break genes” in pathogenic fungi —intentionally inactivating specific genes to determine their functions. The team in his lab also uses CRISPR systems to add fluorescent tags, enabling real-time visualization of gene activity and fungal behavior.
One major focus of the lab is Aspergillus fumigatus, a fungal pathogen responsible for serious infections, particularly in immunocompromised individuals. By generating and studying fungal mutant strains using CRISPR, Dolan’s team investigates how Aspergillus responds to infection-relevant stressors and antifungal treatments.

“CRISPR has allowed us to move beyond the well-adapted lab strains we used to rely on. Now we can edit genes in pathogens taken directly from patients or the environment to better understand how they survive and cause disease,” he said.
In one experiment, the team grows the fungus in the presence of an antifungal drug to identify which genetic changes enable it to keep growing and develop resistance.
“We look at which genes turn on to help the fungus fight back against antifungals. Then we knock those genes out to see if it can still resist—basically testing whether the same story plays out again,” he said.
The rates of Aspergillus and other fungal infections are rising, especially for immunocompromised individuals. Dolan focuses on why individuals with conditions such as cystic fibrosis, those undergoing chemotherapy or with other immune deficiencies are more susceptible to infection.
Dolan hopes to uncover the genetic factors that allow fungi to thrive at infection sites, determine why Aspergillus infects at such high rates and ultimately apply those insights to develop better therapeutic strategies.

Jennifer Mason
Costs and efficiency once limited human genetics research. Now, because of CRISPR, human cancer research has grown rapidly.
Jennifer Mason, an associate professor in the Department of Genetics and Biochemistry, studies how cells respond to DNA damage, including damage caused by sunlight exposure.
The body repairs DNA damage, which is essential to prevent cancer because misrepair leads to the accumulation of DNA mutations.

Mason obtains cancerous and non-cancerous cell lines from human patients and predicts the genes essential for that DNA repair. She then uses CRISPR-Cas9, an enzyme, to knock the gene out. Once the gene is knocked out, she monitors a mutant or knockout cell line to see if the cell can still repair DNA damage.
Mason also works on drug screens to identify compounds that cause a lethal amount of DNA damage to particular cancer cells to find effective targets for chemotherapy. A problem with many compounds that target proteins is that they hit multiple targets and pose issues to non-cancerous cells, so it’s crucial to find a specific target that primarily impairs cancerous cells to mitigate chemotherapeutic side effects. The ease of CRISPR to generate knockouts allows researchers to determine which target of the compound is leading to the observed response.
The burgeoning use of CRISPR started when Mason was halfway through her postdoctoral fellowship at the University of Chicago. Before CRISPR, many DNA repair experiments that make specific changes or knockouts would not have been feasible due to cost and time.
“I got my Ph.D. in human genetics in 2010, and we were limited to the availability of patient cell lines where patients with these disorders consent to having skin biopsies taken,” Mason says.
Many DNA repair disorders and types of cancer arise due to rare mutations. Still, it’s not just one mutation that’s important to understand, but all the different mutations that play a role in tumor propagation. CRISPR allows for testing these specific mutations in non-cancerous cells to understand their individual effect.
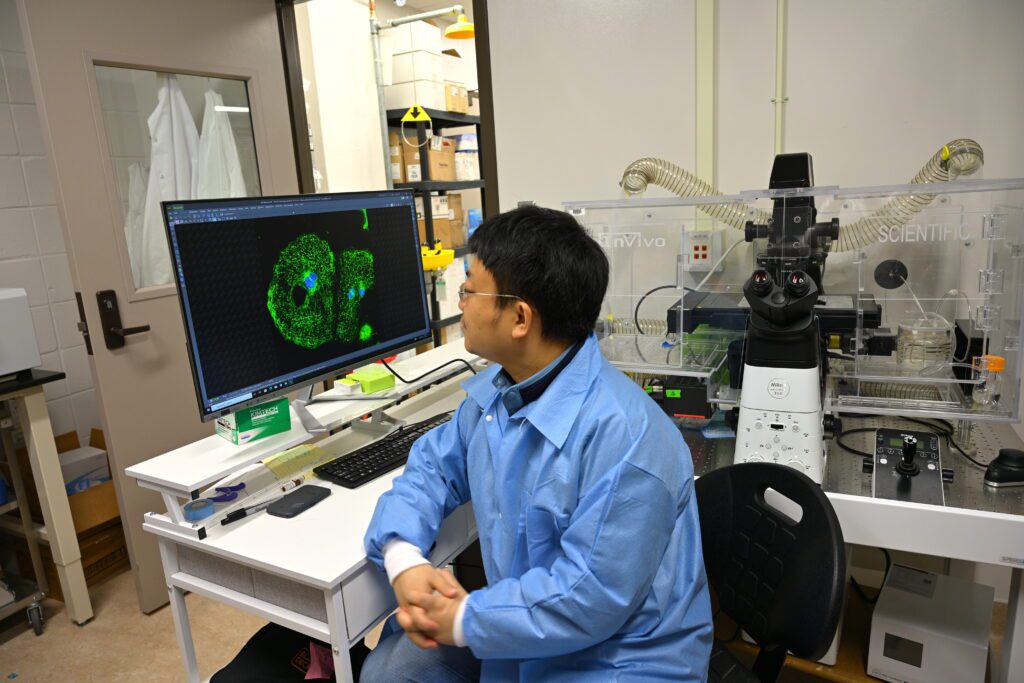
Qing Liu
Qing Liu, an assistant professor in the Department of Biological Sciences, uses human stem cells to understand cardiovascular metabolism and toxicology.
DCas9 is a special version of the Cas9 protein that can stick to a specific spot on DNA but doesn’t cut it. Scientists attach other useful proteins to dCas9 so they can turn genes on or off without changing the actual DNA sequence. This lets researchers control gene activity in a powerful but reversible way, instead of permanently editing the DNA.
Traditional CRISPR uses one guide RNA to target a single gene. Liu’s method, known as CRISPR screening, uses many guide RNAs all at once to identify genome-wide targets. Using bioinformatics, he can determine the critical gene targets and pathways responsible for regulation of cellular metabolism. Since stem cells can develop into many cell types, this method provides a comprehensive framework to uncover novel metabolic regulators. Liu and his team use this system to screen drugs and toxins that affect metabolism.
“The goal of our research is to fill knowledge gaps in our understanding of the mechanisms of cardiac and metabolic dysfunction due to transcriptional dysfunction or chemical exposure, and also, in the future, to benefit predictive developmental biology and toxicology concerning human health,” he said.








