Clemson researchers pursue cutting-edge science and targeted medicine to improve not just lifespan but quality of life.
In the last 25 years, rigorous research, broad medical collaborations and lifesaving interventions have made huge strides for cancer treatment. That means survival rates are up across the board for almost all forms of cancer, including the two most common ones for South Carolinians: breast and prostate cancer.
Title
As recently as the late 1990s, there were clinical trials, and there were heroic efforts, but there were very few effective treatments for combatting some of the most highly aggressive forms of cancer. Twenty-five years later, some of those same cancers have a more than 80 percent survival rate.
Clemson can point to health innovation through research that has played notable roles in improving health outcomes for patients statewide. And that’s because cancer intervention isn’t isolated to bedside care from a nurse or petri-dish analysis from the lab.
Today, cancer treatment is:
- Powered by huge data sets that build the artificial intelligence needed to identify root causes of and precision cures for cancer.
- Innovative approaches, such as precision radio frequency that targets cancer cells rather than an IV drip administering chemotherapy drugs.
- Cellular research to develop new methods of finding and eliminating cancer faster, more safely and more efficiently.
- Identifying and preventing the side effects of treatment drugs and improving quality of life for patients even as they and their health care teams aggressively fight cancer.
Here are some of the Clemson professors contributing research to these lifesaving interventions. A glimpse of their work offers a window into some of the innovations leading the way in cancer treatment.
Targeting cancer with precision
Genetics are the foundational part of what distinguishes one human being from another. There are millions of variants contained in a single genome.
Understanding cancer, at least in part, begins with understanding how genetic variants contribute to the disease. More than 90 percent of trait-associated genetic variants are in non-coding regions that don’t encode any protein-coding genes but may still have regulatory functions.
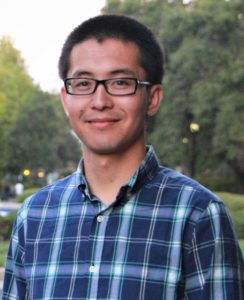
That’s where genetics and biochemistry Assistant Professor Zhana Duren comes in — he performs gene regulatory analysis from single-cell genomics data.
90%
More than 90 percent of trait-associated genetic variants are in non-coding regions that don’t encode any protein-coding genes but may still have regulatory functions.
It’s research that has proven a key contributor to cancer immunotherapy, one of the most cutting-edge cancer treatments available.
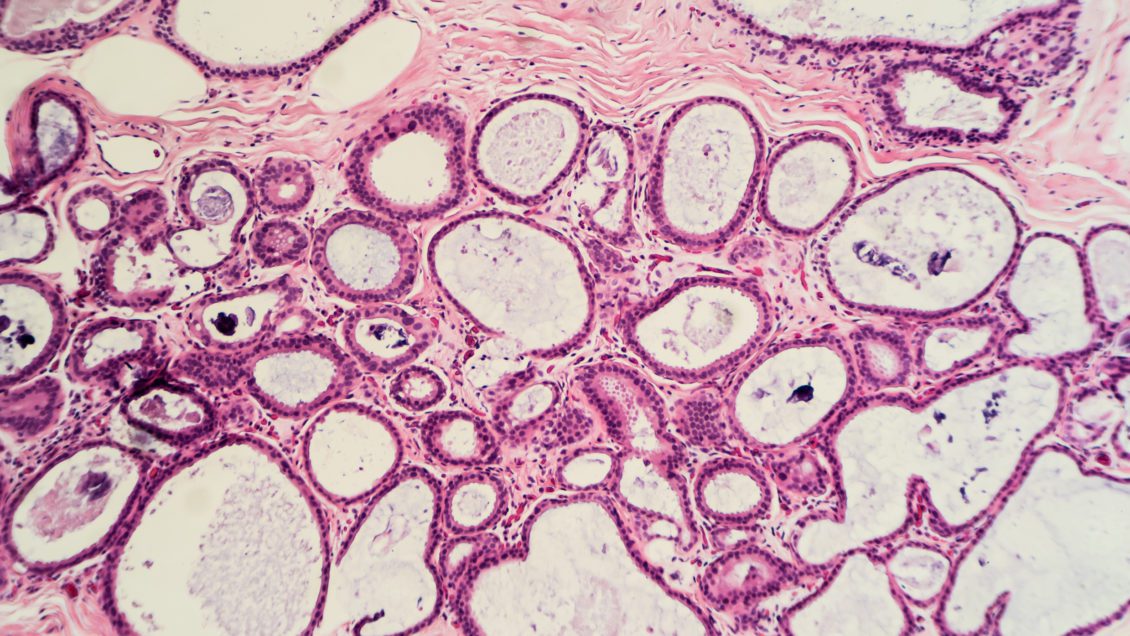
The foundation for immunotherapy research is cellular: Cancer patients have a mixture of normal cells and tumor cells, and traditionally, these cells are analyzed from bulk data. So, a mixture of different cell types is always present. But that makes it difficult to determine the difference between tumor cells and normal cells.
The TOX gene has been identified as a key regulator of T-cell exhaustion. Clemson researchers discovered that one of its paralog genes, TOX2, is the key regulator of tumor-specific B-cell subpopulation. These highly accurate results can improve researchers’ understanding of immune cells and how those cells work.
“By increasing our system-level understanding of cancer, our gene regulatory analysis work has potential application in cancer treatment,” Duren says.
Immunotherapies are one of the most promising cancer treatment methods currently in development. Immunotherapy treats cancer by stimulating or suppressing the immune system in both general and targeted ways, and that can help the body fight cancer, infection and other diseases.
But the main barrier to immunotherapy’s success is “exhaustion of immune cells,” which means that due to chronic stimulation, immune cells simply don’t work as well. Duren’s research group is working to better understand this immune cell exhaustion. And the implications of their cellular-level findings are broad because they can be applied to almost any kind of cancer.
“Our research is about method development,” Duren says. “So, our findings could be applied for many types of cancers and their related treatments.”
The new survival story – growing up with cancer

Childhood and adolescent cancer are considered rare, and yet they still are the leading cause of death by disease past infancy among children in the U.S., according to the National Cancer Institute. Each year, 16,300 children and teens are newly diagnosed with cancer, and they —along with the nearly half a million childhood cancer survivors — don’t just have cancer; they live with cancer.
Associate Professor of Nursing Janice Withycombe wanted to gain a better understanding of what that growing percentage of cancer survivors copes with. Namely, she wanted to understand: What does it feel like to be a young cancer patient?
“Understanding the way clinical trials and treatments affect young patients is complicated,” Withycombe explains. Clinicians — those in the health care system — tend to underrate the severity and frequency of symptoms that children have during therapy.
But children’s caregivers generally overrate those symptomatic experiences, she says.
“The best source for what a patient is feeling is the patient,” Withycombe says. That’s why she is part of a group of national researchers developing a child-friendly system that allows some of the nation’s youngest patients to report their symptoms rather than taking the word of doctors, parents and other caregivers. The first-person data enables clinicians to better care for patients through accurate identification and early intervention for symptom management, ultimately allowing for increased quality of life and uninterrupted delivery of cancer therapy.
She also works with an international group of researchers and clinicians as part of the Children’s Oncology Group. The mission of COG is to cure childhood cancer, and Withycombe is part of a multidisciplinary working group of nurses within the organization pursuing ways to eliminate illness-related distress during childhood cancer. They also provide easy-to-understand educational materials for families of children with cancer — vital work as more and more children live with and survive cancer.
The research program she’s building is related to symptom science and includes physical activity studies in children going through cancer treatment. The goal is to combat symptoms such as fatigue and promote long-term positive health outcomes. Childhood cancer survivors tend to develop chronic illnesses like diabetes, heart disease and obesity, but physical activity can help mitigate these risks.
“My goal is to let children be children and encourage play and physical activity as they go through therapy. I want to help them develop positive habits related to physical activity so they are ingrained within their daily life as they grow older.”
JANICE WITHYCOMBE, ASSOCIATE PROFESSOR OF NURSING
COLLEGE OF BEHAVIORAL, SOCIAL AND HEALTH SCIENCES
Fighting Cancer. Treating patients.

Treating cancer more effectively and with fewer side effects: This is the goal of researcher Angela Alexander-Bryant and her lab that investigates combination drug and gene therapy for treatment of various cancers.
The Clemson Nanobiotechnology Lab is working to develop novel clinically translatable therapeutic delivery strategies to improve targeted treatment of disease. That means leveraging materials science, nanotechnology, gene therapy and drug delivery to advance cancer therapies that lead to cures.
Having new ways of delivering medicines directly to cancer cells raises hopes that, in the future, the disease could be treated more efficiently with fewer side effects than current treatment options.
Though significant progress has been made in the successful treatment of many cancers, there is still a need for further research into strategies to treat cancers with poor prognoses.
ANGELA ALEXANDER-BRYANT, ASSISTANT PROFESSOR OF BIOENGINEERING
COLLEGE OF ENGINEERING, COMPUTING AND APPLIED SCIENCES
Her focus is on cancers that are aggressive and drug resistant such as ovarian cancer. She and her team are creating nanoparticles that would carry nucleic acid-based medicines to cancer cells.
Funded by a $587,676 CAREER award from the National Science Foundation, the research investigates, in part, the barriers nucleic acid-based medicines must overcome to fight cancer. For example, they must get into the cell to be effective, and to do that, they have to be protected from degradation. Alexander-Bryant’s approach is to create nanoparticles made of peptides — sequences of amino acids that are linked by peptide bonds — that are designed to overcome those barriers.
She has created an undergraduate Creative Inquiry research course (Engineering Nanobiomaterials for Delivery of Cancer Therapy) so that even some of the youngest researchers can engage in finding cancer-fighting solutions.
At the high school level, she is creating Project Bioengineering Medicine, an outreach program with hands-on activities to teach students about nanomedicine and biotechnology.
Through research and outreach, she’s growing knowledge and understanding in the lifesaving fight against cancer.
“That’s part of my passion — to do the research,” Alexander-Bryant says. “But also build as I climb to make sure I’m bringing the next generation with me.”
Targeting cancer noninvasively
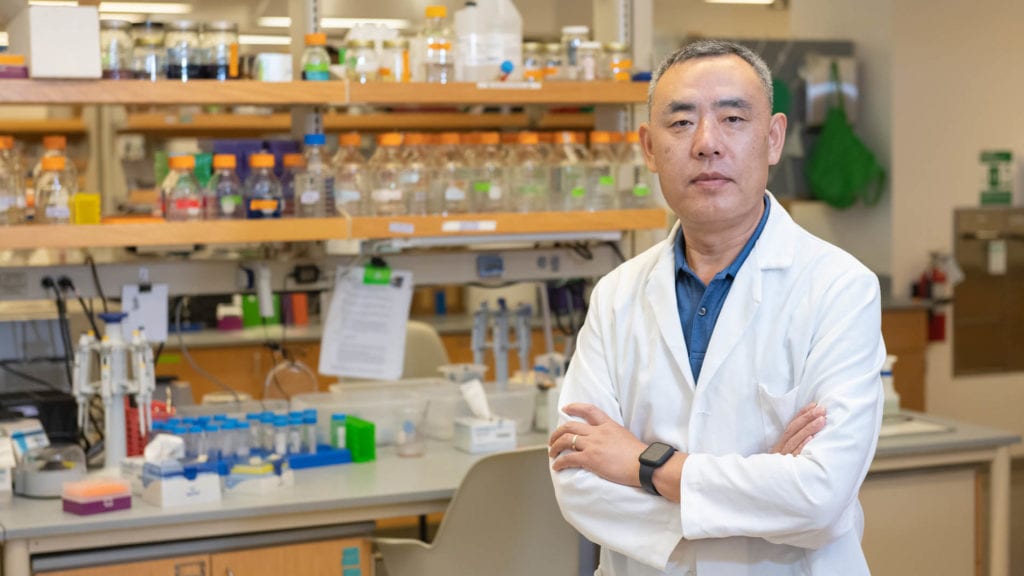
Most breast cancer targeting therapies target one of three receptors: estrogen receptors, progesterone receptors or epidermal growth factor receptors. Professor Yanzhang (Charlie) Wei from the Department of Biological Sciences and his researchers targeted prolactin receptors. Prolactin is a natural hormone in the body and plays a role in breast growth and milk production during breastfeeding. Breast cancer cells overexpress prolactin receptors.
More than 90 percent of breast cancer cells express a high level of prolactin receptors, including one of the most aggressive forms of breast cancer cells: triple-negative. Wei and his team developed a bifunctional protein: One part is a mutated form of prolactin that can still bind to the prolactin receptor but blocks signal transduction that would promote tumor growth; the other part is an extracellular domain of major histocompatibility complex class I chain-related protein (MICA).
When the MICA binds to its receptor NKG2D, it activates the natural killer cells. These natural killers are part of the human immune system, and their targets include tumor cells. It’s a novel approach to developing breast cancer-specific immunotherapy and could lead to new treatment options for the world’s most common cancer.
Yet another Wei study is developing new immunotherapies for cancer by combining tumor cells with dendritic cells, an important part of the body’s adaptive immune system. That work has led to a dendritoma vaccine that proved effective in melanoma, renal cell carcinoma and neuroblastoma patients.
The vaccine was patented and licensed to three biotech companies; two companies are still pursuing the vaccine therapy or related therapy.
Treatment without side effects
It seems counterintuitive that someone who studies electrical and computer engineering would be putting forward research that one day might be a cure for cancer.
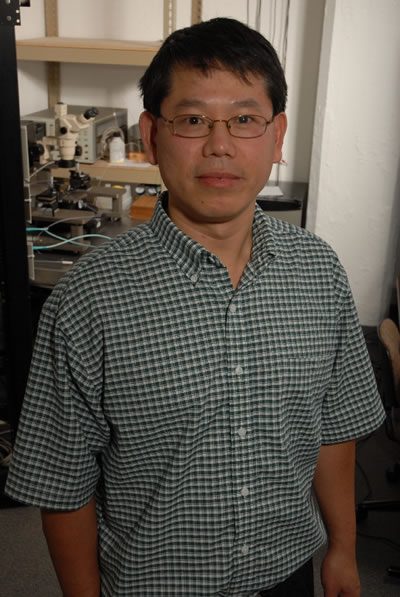
But that’s exactly what Professor Pingshan Wang from the College of Engineering, Computing and Applied Sciences is doing.
Partnering with Professor Charlie Wei, the two researchers are working to find better ways of treating cancer and caring for patients who have the disease.
They are working on a separate cancer-fighting project: to develop noninvasive and precision radio frequency (RF) techniques for side-effect-free cancer treatment at point-of-care settings. This research focuses on lung cancers, which are the leading cause of cancer death in men and women.
“Cancer is a leading cause of death in the U.S. and the world,” says Wang.
“Currently available cancer treatments may have many side effects, which are often linked to damaged healthy cells.”